Le diabète peut être responsable de plusieurs maladies oculaires :
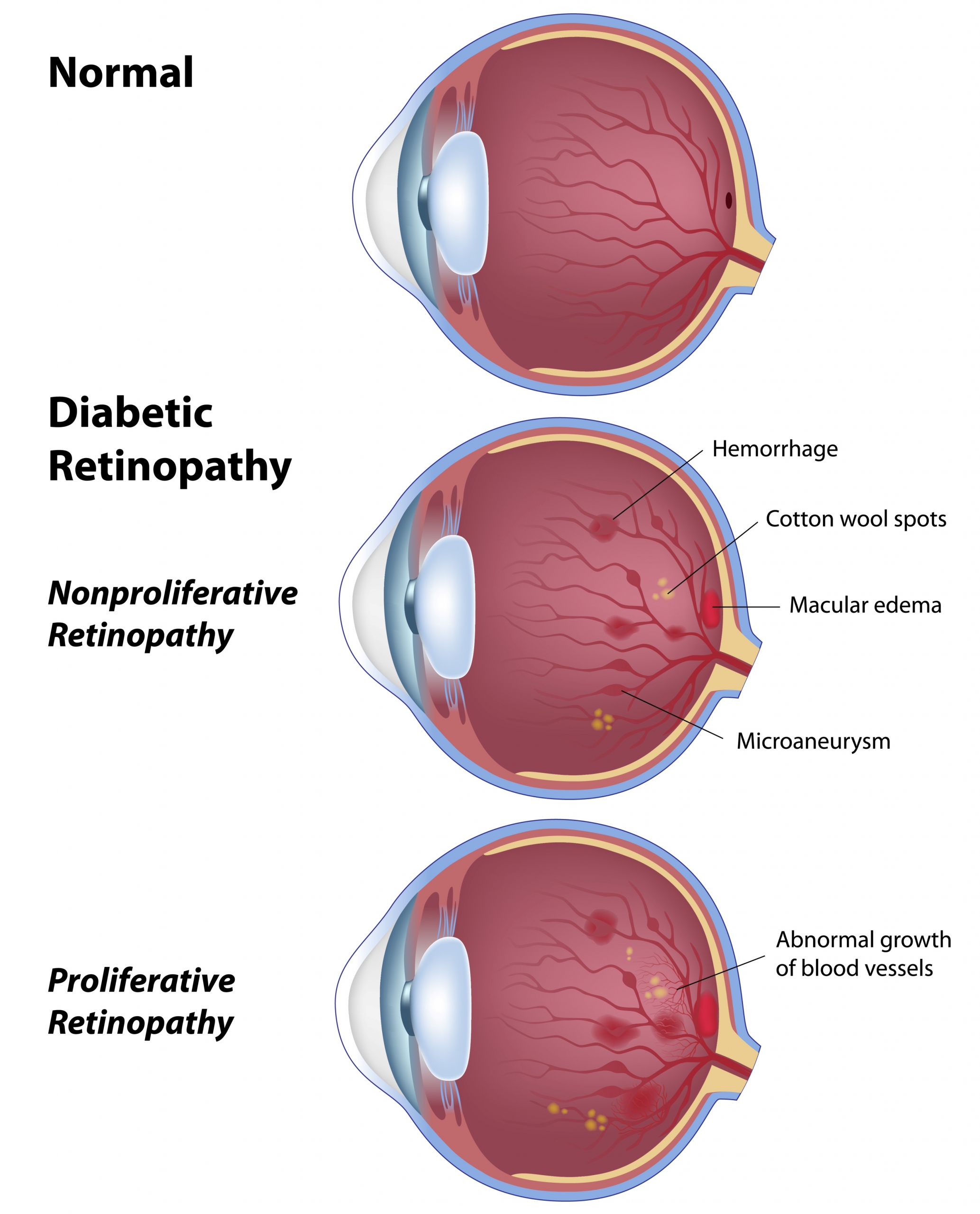
Rétinopathie diabétique : les capillaires de la rétine sont endommagés et permettent l’échappement de fluides qui peuvent affecter la vision (œdème maculaire diabétique). De nouveaux vaisseaux sanguins anormaux peuvent également se développer (rétinopathie proliférante) et mener, en l’absence de traitement rapide, à la cécité.
Cataracte : l’opacification du cristallin de l’œil entraînant une baisse de la vision est beaucoup plus courante et se manifeste plus tôt chez les personnes atteintes de diabète que chez les autres.
Glaucome : cette lésion du nerf optique tend à apparaître prématurément chez les personnes diabétiques.
Neuropathie optique ischémique antérieure : interruption brutale de l’approvisionnement du nerf optique en sang provoquant une déficience visuelle majeure (similaire à une attaque du nerf optique).
Kératopathie : lésions chroniques de la cornée provoquant irritation, rougeur, sécheresse oculaire, larmoiement et, parfois, une baisse de la vision.
Paralysie des muscles oculaires : interruption de l’approvisionnement en sang des nerfs responsables du contrôle des mouvements des deux yeux, avec pour conséquence une vision double.
Occlusion vasculaire rétinienne : obstruction soudaine des artères ou des veines de la rétine, entraînant parfois une déficience visuelle majeure.
Un suivi régulier est important puisque la plupart des effets du diabète sur l’œil ne causent pas de symptômes avant qu’ils ne soient très avancés.
La plupart des déficiences visuelles majeures dues au diabète sont évitables en respectant quelques recommandations :
Maintenir le taux de glyceémie HbA1c le plus près possible de la normale : une valeur autour de 6 % réduit considérablement le risque de développer des complications oculaires.
Maintenir un bon contrôle de la pression artérielle par l’alimentation, l’activité physique et la médication
Améliorer le profil lipidique sanguin par l’alimentation, l’activité physique et la médication
Cesser de fumer : le tabac rétrécit les vaisseaux déjà fragilisés.
Effectuer régulièrement un examen de l’œil dilaté chez un ophtalmologue : un diagnostic précoce et un traitement approprié permettent d’éviter la plupart des cas de déficience visuelle grave.
Traitement
La rétinopathie diabétique proliférante est traitée par photocoagulation panrétinienne (PPR) au laser. Le traitement est réalisé en ambulatoire après l’application de gouttes anesthésiantes. Il faut prévoir en général plusieurs séances. Cette intervention permet d’obtenir la régression des néovascularisations dans la plupart des cas et de réduire considérablement le risque de cécité.
La maculopathie œdémateuse est aujourd’hui traitée par injections intravitréennes « anti-VEGF » dans l’immense majorité des cas. Lucentis® (ranibizumab) et Eylea® (aflibercept) sont les médicaments les plus utilisés. L’injection est réalisée en ambulatoire après l’application de gouttes anesthésiantes et ne dure que quelques secondes. Plusieurs injections sont nécessaires pour traiter l’œdème maculaire diabétique durant plusieurs années.
L’injection intravitréenne de corticoïdes est indiquée chez certains patients. La durée moyenne d’efficacité des corticoïdes est de quatre à six mois, ce qui permet de réduire le nombre d’injections.
La photocoagulation focale au laser était pendant longtemps le seul traitement disponible de l’œdème maculaire diabétique. Il peut aujourd’hui encore être indiqué chez certains patients.
Nous prenons en charge l’ensemble des maladies de l’œil,
du diagnostic initial au suivi régulier.