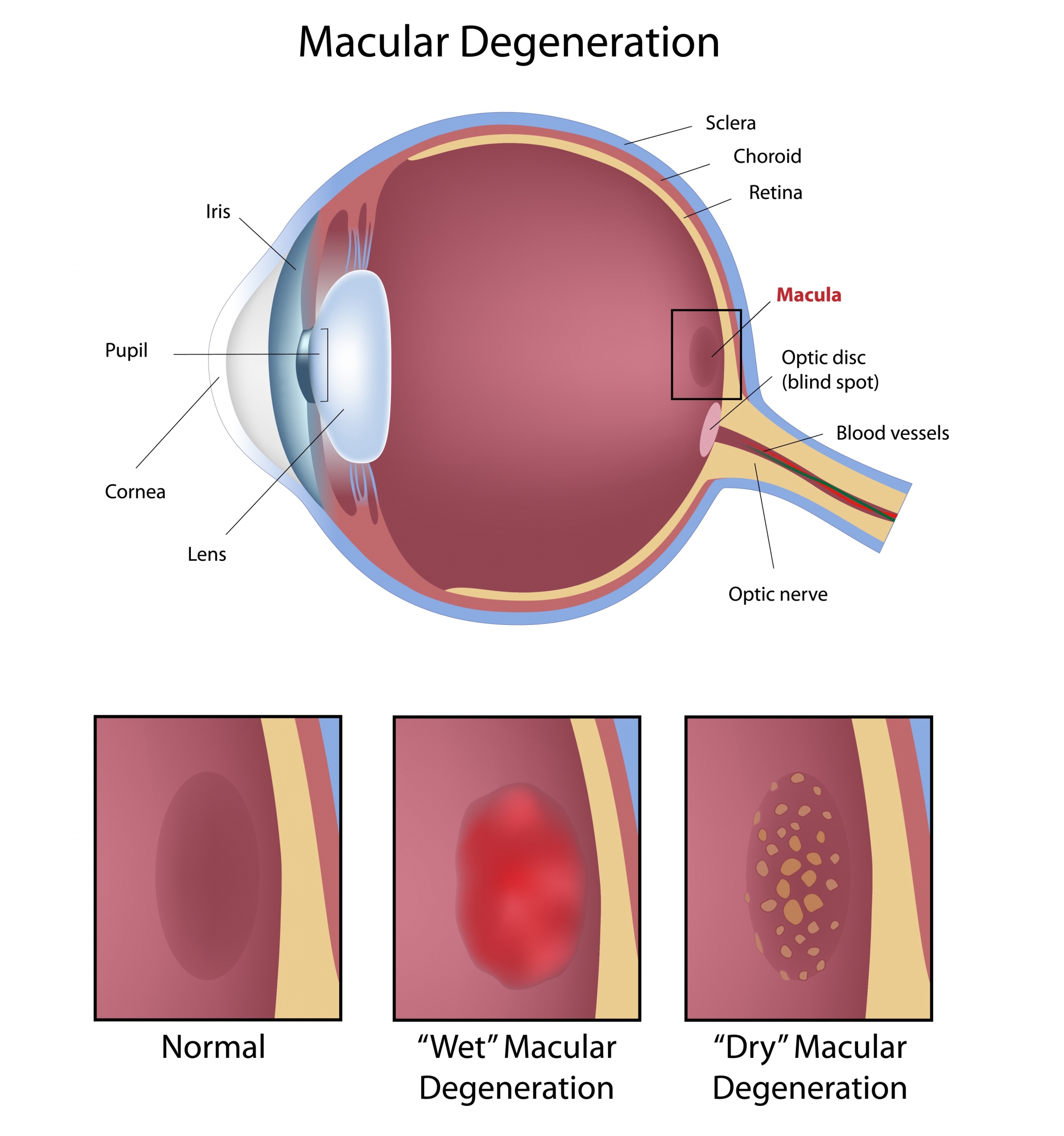
The retina is the sensitive organ of vision. It is a thin membrane covering most of the inner surface of the eyeball. This neurosensory tissue contains highly specialized cells, photoreceptors, and picks up light rays. The visual information is then transmitted to the central nervous system.
The macula, also called yellow spot, is an area of the retina located at the back of the eye.
It contains the fovea centralis, the place where visual acuity is best.
MACULAR DEGENERATION
Macular degeneration results from the deterioration of the macula. It involves a gradual loss of central vision, which becomes increasingly blurry, as well as distortion of objects (straight lines become distorted).
Macular degeneration mainly affects people aged 55 and over.
It is then called age-related macular degeneration or AMD
There are two forms of AMD: dry AMD, also called atrophic, is the less serious and more frequent form. It evolves slowly over several years. All age-related macular degeneration begins in the dry form before progressing in about 10% to 15% of patients to the wet form. Wet AMD, also called exudative or neovascular, is therefore an exacerbation of the dry form. It is characterized by the formation of new blood vessels in the choroid, under the retina. Fluid build-up causes vision loss faster than the dry form. The wet form can lead to complete loss of central vision.
No one is safe from age-related macular degeneration (AMD), but there are factors, some controllable and others not, that increase the risk of AMD. Some uncontrollable risk factors include age, family history, and Caucasian race. On the other hand, lifestyle habits play an important role, smoking being one of the main risk factors. Do not neglect a healthy diet rich in omega-3 (nuts, cold water fish, flaxseed and rapeseed oil), as well as physical activity and weight control. It is also important to control blood pressure and protect your eyes from UV rays.
Treatment
To date, there is no cure for atrophic AMD.
In some cases, vitamin supplements in a specific formulation called “AREDS” can reduce the risk of vision loss and progression.
The treatment of wet AMD is currently based on “anti-VEGF” drugs of which Lucentis® (ranibizumab) and Eylea® (aflibercept) are the most widely used. These drugs help stabilize the vision of the vast majority of patients treated, and even improve visual acuity. Giving these drugs directly into the eye has the advantage of very effective local action while minimizing systemic side effects. The intravitreal injection is done on an outpatient basis after applying anesthetic drops and only lasts a few seconds. The medicine is injected with a very fine needle through the sclera (white of the eye). This injection is safe for nearby eye structures.
While these injections can stabilize or even reverse the disease, they cannot cure it permanently. They must therefore be repeated often.
Retinal detachment
Retinal detachment is a potentially dangerous condition. In general, people of middle or advanced age are affected; more myopic. Most often, retinal detachment is caused by a tear in the retina, but it can also occur after a blow to the eye or have other, rarer causes. If not treated quickly, retinal detachment can cause vision loss or even loss.
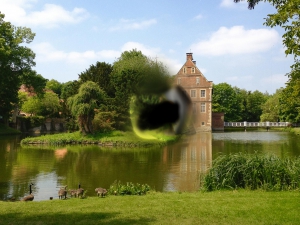
Early signs
The sudden appearance of dark spots in the visual field (flying flies or soot rain), flashes of light not provoked by an obvious cause or a dark shadow on the periphery of the field of vision can announce a detachment of the retina. A decline in vision is a later sign. From the outside a protruding retina is not visible and the affected eye is neither red nor painful.



In the presence of any of these symptoms, it is therefore imperative to consult an ophthalmologist as soon as possible.
Treatment
If the retina is torn, but little or little detached, prompt laser treatment can prevent the detachment. This treatment is performed on an outpatient basis after the application of anesthetic drops
If on the other hand the retina is detached, the treatment consists in a surgical intervention.
OPHTHALMOLOGY CENTER
Ophthalmological consultation and treatment center located next to Place de Paris, in Luxembourg.
Dr Christian Eulufi
Dr Tom Pavant
Dr Carla Schmartz
Dr Philippine Delvaulx
Dr Mihaela Dilion
USEFUL INFORMATION
34, avenue de la Liberté
L-1930 Luxembourg
Opening time
Monday, Tuesday, Thursday and Friday: 8 a.m. to 12 p.m. and 1:30 p.m. to 5 p.m.
Wednesday: 8 a.m. to 12 p.m.
MAKE AN APPOINTMENT
By phone at +352 28 86 72
Monday to Friday 8 a.m. to 12 p.m. and 1:30 p.m. to 3 p.m., except Wednesday afternoon
By email by writing to [email protected]
Comprehensive care for the patient