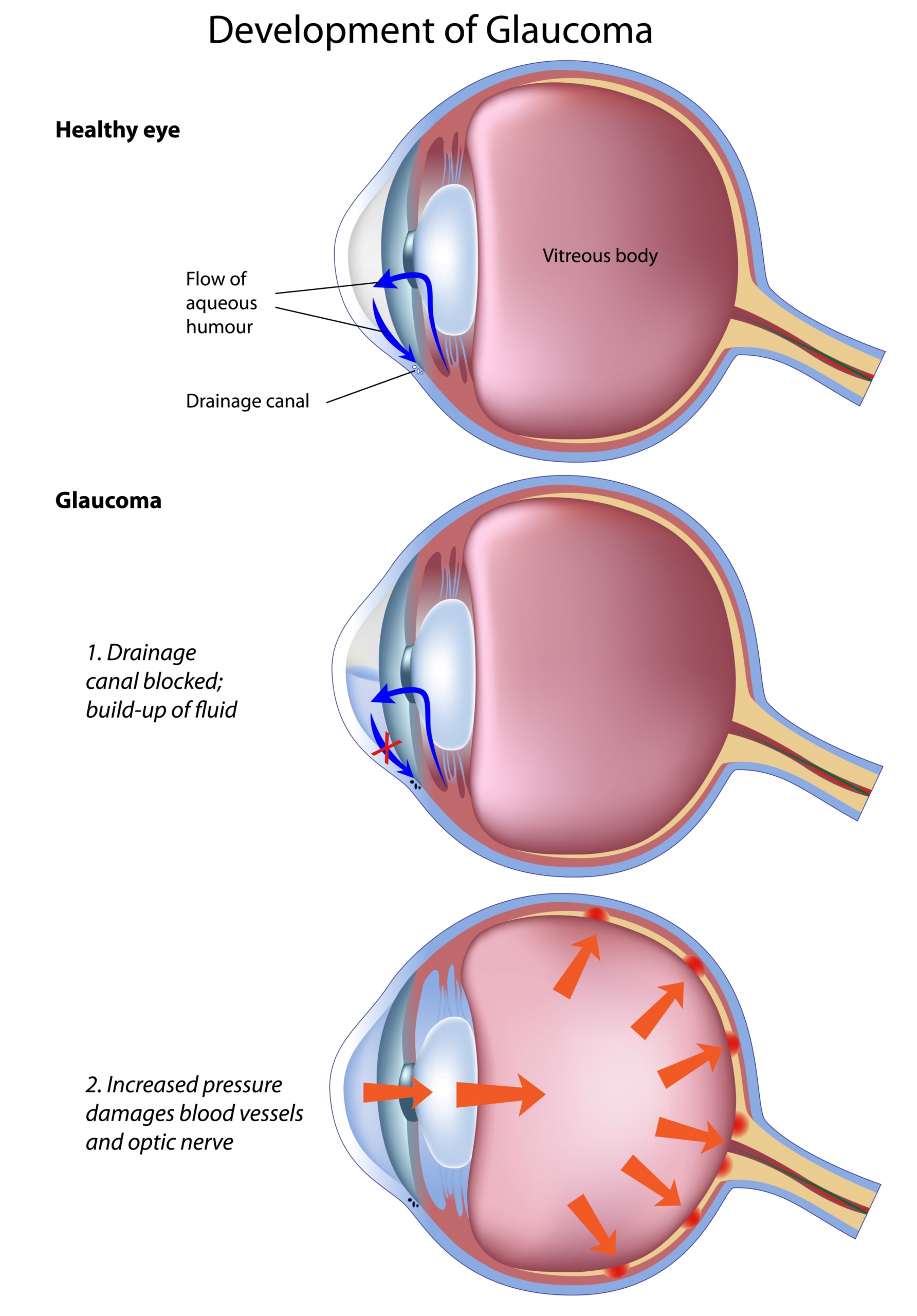
Glaucoma is a chronic, irreversible disease which gradually destroys the nerve fibers in the optical nerve, causing damage to the field of vision. In most cases, the field of vision begins to deteriorate in the peripheral areas, causing the “tunnel vision” phenomenon.
The disease may stem from various causes, the most significant risk factor being elevated intraocular pressure.
Intraocular pressure is the result of the speed at which aqueous humour (the transparent liquid which enables the eye to maintain shape) is produced, coupled with the rate at which it drains.
There are various forms of glaucoma, classified according to physiopathology.
Notably, a distinction is made between primary and secondary glaucoma, as well as between open-angle and closed-angle glaucoma. The majority of patients (>90%) present a primary, open-angle glaucoma. This disease affects about 2% of the population over age 40, and is one of the primary causes of blindness in the world.
Glaucoma and intraocular pressure
Elevated intraocular pressure does not always lead to glaucoma, because optic-nerve susceptibility differs from person to person. Ocular hypertension is defined as increased intraocular pressure in the absence of any optic nerve lesion. Only the ophthalmologist knows whether ocular tension should be treated or not. However, even if treatment is not (yet) necessary, regular check-ups are indicated.
Conversely, glaucoma may be present even if the intraocular pressure measurement is normal. Some individuals have such a vulnerable optic nerve that they develop glaucomatous damage even with ocular pressure within the range of statistically normal (this is called “normal pressure glaucoma”). The ophthalmologist alone can detect changes in the optic nerve, prescribe the appropriate tests, and establish a treatment regimen.
Symptoms




Glaucoma is a silent disease. The patient does not perceive the damage the disease has done to his or her vision until it is at an advanced stage.Only the ophthalmologist is capable of detecting the first signs, by examining the optic nerve and by requesting additional examinations, like a visual field test.Because damage to the optic nerve is irreversible, glaucoma screening should not be postponed.
Risk factors
a family history of glaucoma
age: the incidence of glaucoma increases over age 40
being darker-skinned
steroid use (recently or earlier in life)
high blood pressure and cardiovascular diseases
low blood pressure (iatrogenic, nocturnal, or orthostatic)
sugar diabetes
strong myopia
vasospasms (Raynaud’s syndrome, migraine)
Methodes of examination
dilated fundus examination: examination of the optic nerve and cupping
intraocular pressure measurement: 15 mmHg mean value in adults
visual field test: shows early damage from glaucoma
OCT of the optic nerve head: measures thickness of optical fibres
HRT: measures size and depth of optic nerve cupping
gonioscopy: examines the angle in the eye where the iris meets the cornea to determine glaucoma type
pachymetry: measures the thickness of the cornea to evaluate pressure measurements
Treatment
The goal of treatment is to stabilize the disease in order to preserve eyesight, by reducing intraocular pressure.
Generally, drops aimed at lowering pressure are prescribed as first-line treatment, but laser treatments or surgery may be indicated from the very beginning.
Today, most cases of glaucoma can be managed, as long as the patient has regular check-ups and follows the ophthalmologist’s instructions.
Medication: treatment is usually based on the administration of eye drops. Oral medication is much rarer. There are many brands of eye drops that lower ocular pressure. They may act to reduce the production of aqueous humour, or facilitate its draining.
Laser: there are various types of laser, appropriate to various types of glaucoma.
Chirurgie : urgery is not usually necessary unless the disease is progressing despite medication or after laser treatment. There are several surgical techniques.
Prevention
Early detection is vital, and is the ophthalmologist’s duty. Every patient over the age of 40 should regularly undergo tests of intraocular pressure.
Once the diagnosis has been established, it is important to apply the eye drops regularly, without gaps in the treatment, and to respect the exam schedule setup by the ophthalmologist.
OPHTHALMOLOGY CENTER
Ophthalmological consultation and treatment center located next to Place de Paris, in Luxembourg.
Dr Christian Eulufi
Dr Tom Pavant
Dr Carla Schmartz
Dr Philippine Delvaulx
Dr Mihaela Dilion
USEFUL INFORMATION
34, avenue de la Liberté
L-1930 Luxembourg
Opening time
Monday, Tuesday, Thursday and Friday: 8 a.m. to 12 p.m. and 1:30 p.m. to 5 p.m.
Wednesday: 8 a.m. to 12 p.m.
MAKE AN APPOINTMENT
By phone at +352 28 86 72
Monday to Friday 8 a.m. to 12 p.m. and 1:30 p.m. to 3 p.m., except Wednesday afternoon
By email by writing to [email protected]
Comprehensive care for the patient